A lung transplant recipient presents with progressive dyspnea and Severe Anemia. Explore the diagnostic challenge of pure red cell aplasia in this case.
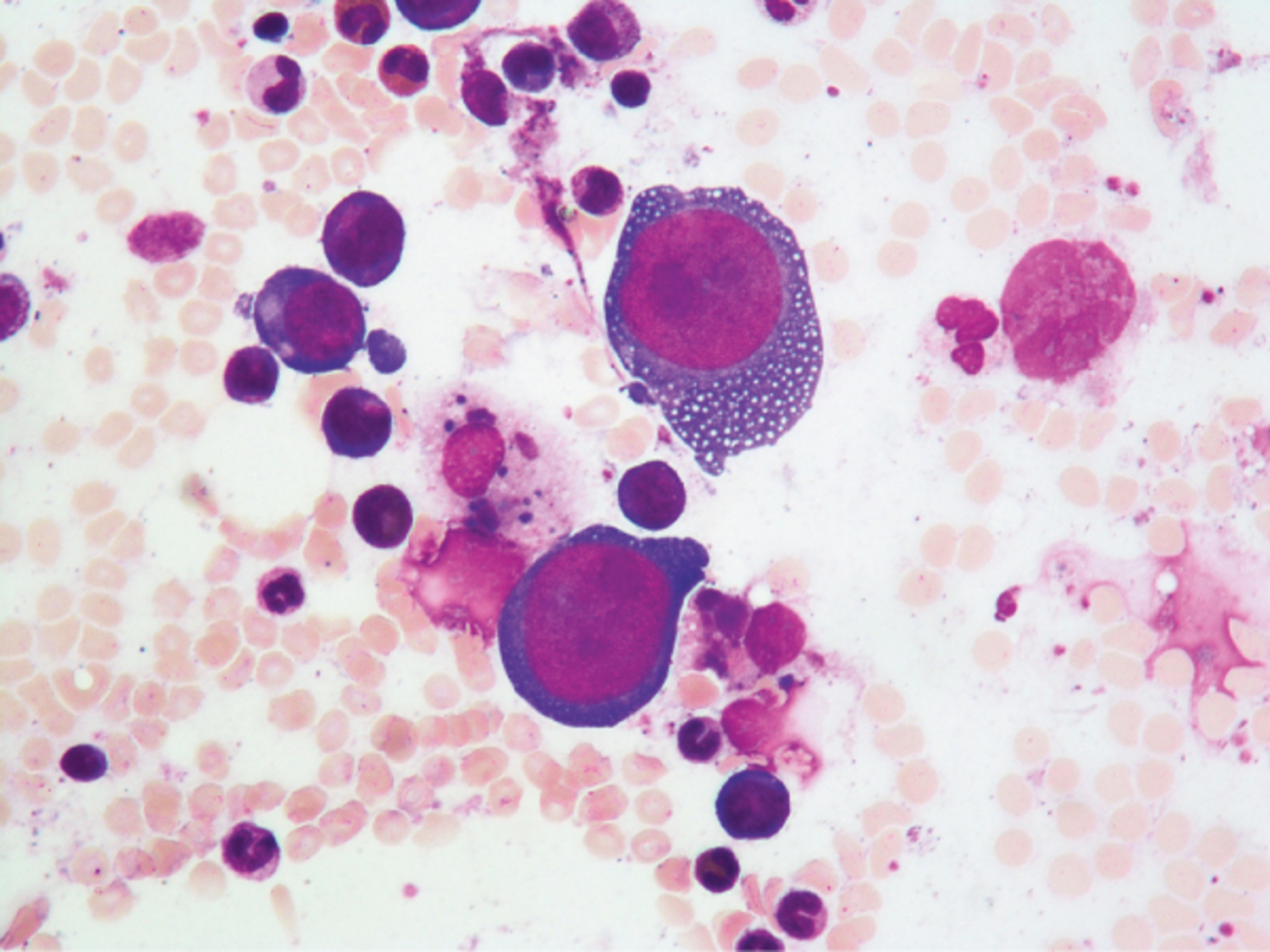
A 67-year-old woman presented to the emergency department with a 6-week history of progressive exertional dyspnea. Her medical history was notable for lung transplantation that had been performed 8 years earlier. Laboratory studies showed normocytic anemia, with a hemoglobin level of 6.9 g per deciliter (reference range, 11.9 to 17.2). White-cell and platelet counts were normal. The reticulocyte index was 0%. Bone marrow aspiration was performed and showed giant proerythroblasts with basophilic and vacuolated cytoplasm, uncondensed chromatin, and large, intranuclear, purple-colored inclusions. What is the diagnosis?
What is the most likely diagnosis?
Anemia, Giant proerythroblasts, Immunosuppression, Parvovirus B19 infection, Pure red cell aplasia